“Community pharmacy has come to a point where we have to change ourselves,” said Raj Matharu, CEO at Community Pharmacy South East London, and Superintendent Pharmacist of Westchem Pharmacy, as he opened a panel discussion at the recent Pharmacy Business Conference.
The 'Optimising Service Opportunities' session centred on how community pharmacies can safely and profitably deliver high-quality NHS and private services, while ensuring an excellent patient experience.
Patricia Tigenoah-Ojo, superintendent pharmacist at Stevens Pharmacy, highlighted the importance of diversifying services beyond NHS services.
“I'm not new to change,” said Patricia Tigenoah-Ojo, who has three decades of experience across acute, primary, and community care as a dual-registered pharmacist and nurse.
When she became a pharmacy owner just two months before the COVID lockdown, Patricia knew that she needed to offer more than just the NHS services.
As an independent prescriber, she was particularly interested in Travel Clinic, so she decided to focus on expanding her scope of practice in that direction.
While Travel Clinic remains their predominant area, they also offer minor illness services, with plans to continue growing and diversifying the offerings.

Reflecting on the changes she has made in her pharmacy to adapt to today’s demands. She said: “The main thing that I've had to do in terms of navigating the new system is how we take on contact from patients directly in the pharmacy.”
“I’ve made sure that my staff can work in different aspects of the pharmacy, so they're not just restricted to the counter or with the dispensing.
“That's made it very easy to deal with the staffing. I've had the same members of staff, but they've all learned to be able to fit into each other's shoes. This has given us a lot of flexibility.”
Additionally, she has introduced a pharmacy website with a contact form and email support to improve patient engagement. Every staff member is trained to manage queries and escalate issues appropriately.
Marketing services actively is another key strategy that Patricia believes pharmacies should focus on.
“We do have to be able to market ourselves, so everyone understands that when they pick up the phone, the first thing they do is actually introduce what we are – a pharmacy and a travel clinic.”
“Everyone is involved in making sure that we showcase what we can do in the community pharmacy.”
Diversification, agreed Raj, is essential: “You cannot have all your eggs in one basket.”
Harnessing Digital Solutions
Baba Akomolafe, superintendent pharmacist at Christchurch Pharmacy, highlighted the role of technology in optimising patient flow.
He talked about a QR code that he has introduced in his pharmacy to direct patients to the right person or service.
If you arrive at 9am and 10 patients have already walked into your pharmacy, sent by three different surgeries, what do you do? It could take you an hour just to gather all their presenting complaints.
At Christchurch Pharmacy, patients can quickly scan a QR code and complete a form, which is instantly sent to their NHS email and printed on their Brother printer within just three minutes.
Then, their pre-reg picks them up, triages the complaints, and deals with the ones they can. Anything they can't manage gets passed to IP (independent prescriber) working under the IP Pathfinder, or to one of our two clinical pharmacists. If they’re too busy, Baba steps in from head office and picks up the case himself.
“We need to go digital,” Baba said, advocating for a unified QR code for community pharmacies to streamline patient access and service delivery.
When a patient needs to see a pharmacist, they just scan the code, and it will guide them through eligibility criteria — for UTIs, sore throats, and more.
“If we sit here waiting for the NHS to fix us, it's not going to happen. We need to come together,” Baba noted.
Raj echoed the sentiment: “Total triage, just like in general practice, needs to happen in community pharmacy too.”

The power of data
At Day Lewis Pharmacy, technology and data are central to delivering consistent, high-quality services across its 250-strong network, explained Rachna Chhatralia.
“We are increasingly using technology to capture and merge data centrally in its head office. Without this data, our 250 pharmacies would not be able to reach the level that’s expected by the NHS and also by the patients,” said Rachna.
They've developed their own CRM platform to target specific patient groups with tailored advice, suggestions, and services.
Day Lewis also has its own booking and patient feedback system that provides key insights and valuable learning, helping them continuously improve service delivery.
For governance of their services, the group has an internal compliance hub for auditing and training pharmacy teams.
“My team would actually look at the data on this compliance hub, and they will ensure that there's compliance with SOPs processes, and also make sure that the teams are appropriately trained.
Rachna acknowledged the advantage of having data streams and teams for data analysis in a large organisation, but expressed concern about the consistency of services across the sector.
She emphasised the need for an infrastructure to support everyone in the sector with appropriate training and auditing to ensure that service delivery issues are addressed.
“We've lost so many pharmacies to date, and we've just got to make sure that we do support everyone when it comes to service delivery,” she added.

Balancing NHS and Private Services
The experts also stressed the importance of keeping the right balance between NHS and private services.
“At Day Lewis, we have a team who writes our own PGDs — we have a suite of 60. We leave it to the pharmacy teams to decide which private services they want to offer, based on the needs of their local population. However, when it comes to NHS core services, every one of our pharmacy teams delivers all of them,” Rachna explained.
Asked how she divides the time between NHS patients and private patients, Patricia said: “One of the first things I did was train my technician to become an accuracy checking technician. That lifted a huge burden, as final checking was taking up a lot of my time.”
She also focused on upskilling the rest of the team to strengthen the dispensary team, which freed her to focus more on private services.
“Private services aren't the biggest part of our business — we’re still fundamentally an NHS contractor — but they help us stay afloat,” Patricia added.
How do you choose which private services to run with?
“You can't choose which services to offer — patients will tell you what they need,” Baba responded.
Baba emphasised that they had people coming in asking for earwax removal, travel clinic services, and cryotherapy appointments, so they adapted to meet those demands.
What is in your control and what's not?
“The NHS contract funding is not in my control, but balancing the books is,” Patricia said.
She focuses on making better use of existing staff rather than losing them, and using new IT systems like Titan and PharmacyX to improve efficiency, especially around clinical checking.
“We can't invest more than we're receiving, but we can certainly look to the future.”
“So, what’s in my control is using my staff and my time as efficiently as possible and exploring new opportunities.”

Raj concluded: “Optimising services comes from when you decide to make the change and stand up to be a leader within your community pharmacy.”
“Nothing's going to be handed to you. You're going to have to graft for what you need to achieve within your pharmacy.”
He advised focusing on the seven clinical conditions moving forward because “that's what's going to earn you the incentive payments and that is worth more than anything else in terms of return investment within your pharmacy.”










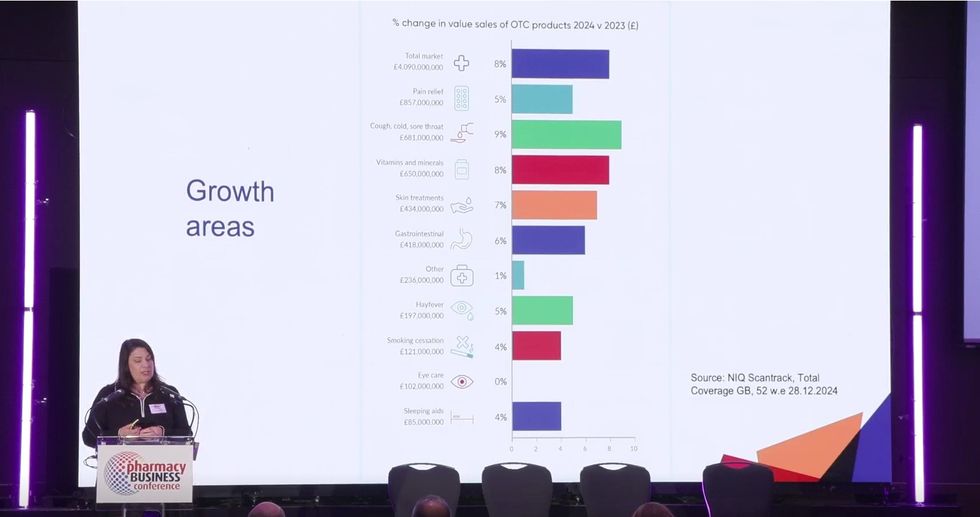 NielsenIQ data shows a positive trend in OTC sales
NielsenIQ data shows a positive trend in OTC sales 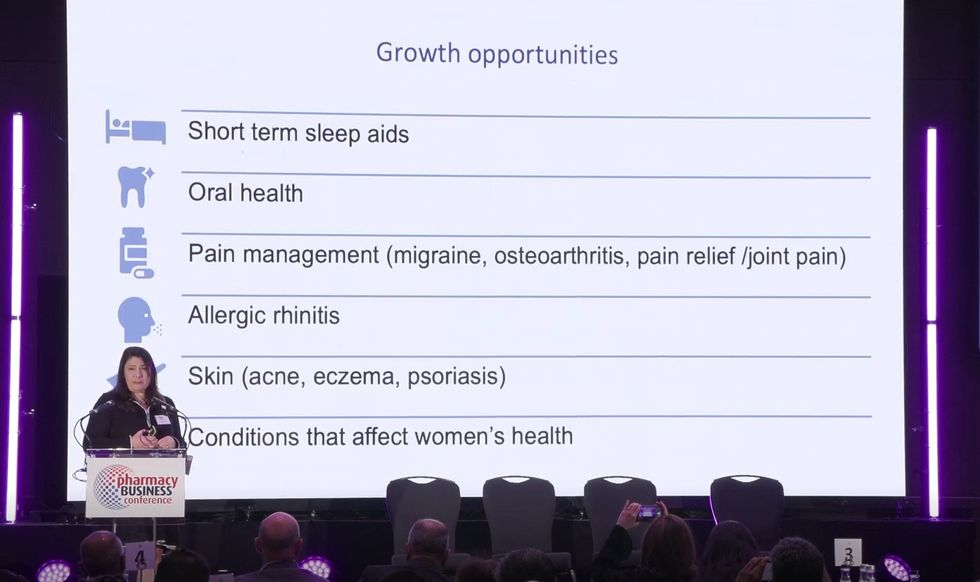 Six broad health conditions where medicines can be reclassified are shown on the screen.
Six broad health conditions where medicines can be reclassified are shown on the screen. 








 Health Secretary Wes Streeting addresses Pharmacy Conference via video
Health Secretary Wes Streeting addresses Pharmacy Conference via video  David Webb, chief pharmaceutical officer of NHS England
David Webb, chief pharmaceutical officer of NHS England Shailesh Solanki, executive editor of Pharmacy Business
Shailesh Solanki, executive editor of Pharmacy Business L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul
L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul  L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu
L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu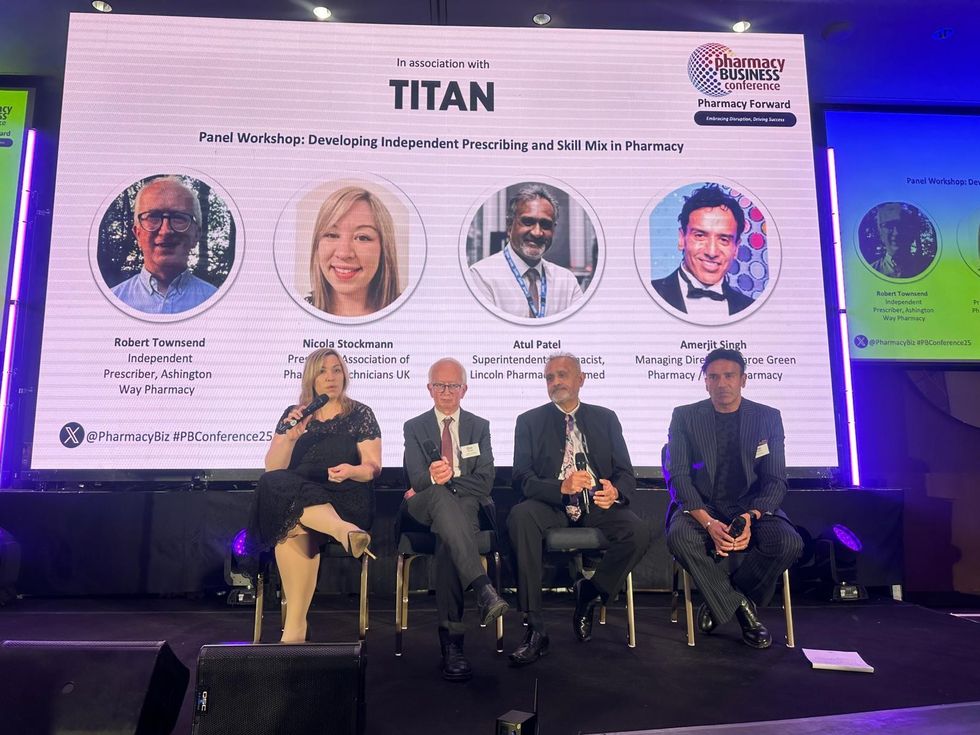 L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh
L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh Wole Ososami, lead pharmacist at Westbury Chemist
Wole Ososami, lead pharmacist at Westbury Chemist