By Harry McQuillan
Chair, Numark
The future of community pharmacy is one built on clinical expertise, expanded services, and a stronger role in preventative and urgent care. As the sector awaits clarity on future funding agreements in England, there is an opportunity to shape a model that aligns with patient needs and the evolving role of pharmacists. Numark’s 12 principles for pharmacy practice offer a clear vision, one that recognises the increasing importance of services coupled to medicines supply.
Pharmacists are highly skilled clinicians, yet their expertise remains underutilised. The future must fully embrace prescribing as a fundamental part of community pharmacy practice. This means enabling pharmacists to manage repeat prescriptions, support long-term conditions, and treat acute and common illnesses with increased autonomy.
For this to happen, funding agreements must prioritise service-led models. A balanced approach must reward patient-facing clinical work, ensuring investment in pharmacist-led prescribing services.
The current contract structures in England have placed immense financial strain on community pharmacies. Future agreements must reflect the reality that pharmacy services are an essential part of the healthcare ecosystem. The principles outlined by Numark advocate for a model where, as funding grows, an increasing proportion is allocated to service delivery.
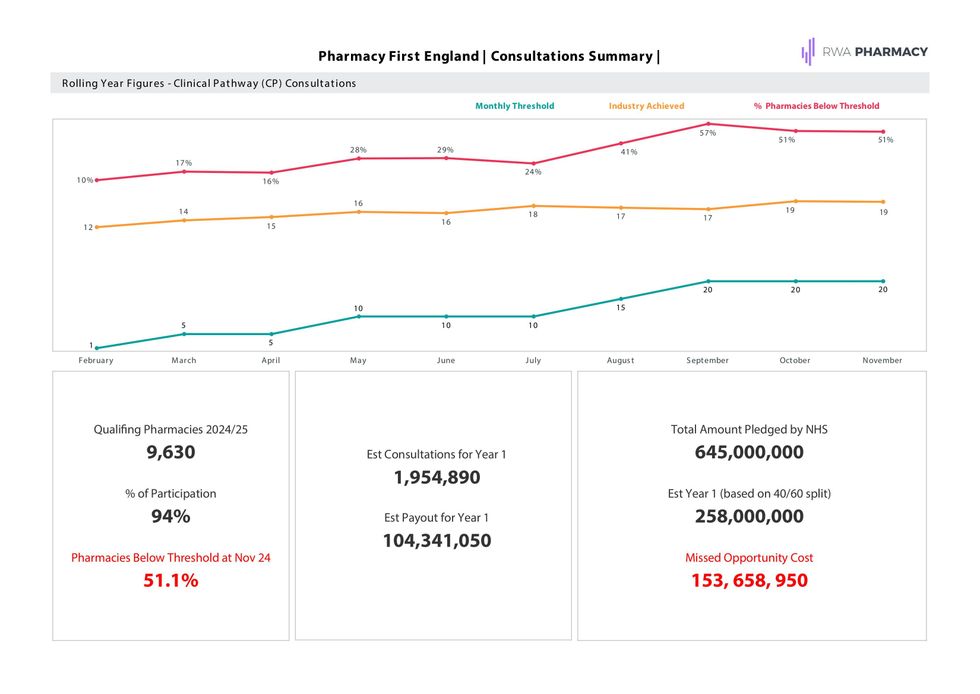
This shift is already visible in Scotland, where the Pharmacy First service empowers pharmacists to provide treatment for minor illnesses without the need for a GP appointment. England must follow suit through the expansion of Pharmacy First conditions.
Funding must also be flexible enough to support emerging services, from vaccinations to long-term condition management, while ensuring core medicine supply remains robust.

One of pharmacy’s greatest strengths is its accessibility. Community pharmacies are often the first point of contact for health concerns, making them ideally positioned to play a larger role in preventative and urgent care.
Future funding agreements must enable pharmacies to deliver health checks, disease prevention initiatives, and urgent care services that aim to ensure the patient receives the right care, in the right place at the right time. A further benefit of this approach is a reduction in the current pressure being experienced by GP surgeries and hospitals. By commissioning structured services, the NHS can leverage pharmacy’s unique strengths to improve population health and reduce long-term healthcare costs.
With the right funding, pharmacists and their teams can support patients in managing common conditions, providing rapid access to appropriate treatments and reducing unnecessary GP and A&E visits. This is not just about convenience; it’s about ensuring that healthcare is accessible where and when patients need it most.
A national approach to commissioning services is essential for patient clarity and confidence. Under the right funding model, all community pharmacies should offer a core set of NHS-funded services, ensuring that patients know what to expect regardless of location.
At the same time, local commissioning must retain some flexibility to address regional health priorities. Regional urban and rural communities face different healthcare challenges, and commissioning structures must allow for tailored service offerings to reflect these needs.
The future of pharmacy hinges on a funding model that recognises and rewards service delivery. Numark’s principles provide a framework for this shift, one that champions clinical expertise, expands service provision, and ensures pharmacy remains a cornerstone of accessible, community-based healthcare.
For England, the long awaiting funding agreement must embrace this reality, creating a system that sustains pharmacies and enables them to thrive as the frontline providers of primary care services. The opportunity is there, it’s time to seize it.









 Wes Streeting outlines ambitious NHS reform plansPic credit: Getty images
Wes Streeting outlines ambitious NHS reform plansPic credit: Getty images Pharmacies played a critical role during the pandemicPic credit: Hollie Adams/Getty Images
Pharmacies played a critical role during the pandemicPic credit: Hollie Adams/Getty Images







 Shivam Modi
Shivam Modi 
 Graham Thoms , CEO and co-owner, Pharmadoctor
gettyimages
Graham Thoms , CEO and co-owner, Pharmadoctor
gettyimages