Sector hopes that the Darzi report will prompt ministers to act swiftly against the chronic underfunding driving pharmacy closures
The Department of Health and Social Care (DHSC) recently published Lord Darzi’s report on the state of NHS England, revealing that the health service is in “serious trouble.”
“The service has been chronically weakened by a lack of capital investment, which has lagged behind other similar countries by tens of billions of pounds,” he stated.
Shortly after taking office, Health Secretary Wes Streeting commissioned an independent investigation to assess the challenges facing the healthcare system in preparation for a new 10-year health plan. Former surgeon Lord Ara Darzi was appointed to lead this review.
In his report, Lord Darzi pointed out that the NHS has failed to meet key promises made to the public since 2015, and patient satisfaction is now at its “lowest ever level.”
Rising waiting times and difficulties accessing GPs were highlighted as major concerns. “There are huge and unwarranted variations in the number of patients per GP, and shortages are particularly acute in deprived communities,” he said.
Lord Darzi described the state of A&E as “awful,” noting that nearly 10% of patients wait 12 hours or more today.
Additionally, Lord Darzi’s investigation found that the NHS budget is not being optimally allocated, stating that “too great a share is being spent in hospitals, too little in the community, and productivity is too low.”
The report identified 4 inter-related factors contributing to the NHS's current dire state: 1) Austerity in funding and capital starvation; 2) The impact of the Covid-19 pandemic and its aftermath; 3) Lack of patient voice and staff engagement; and 4) Inefficient management structures and systems.
“All of this has occurred while the demands placed upon the health service have grown as the nation’s health has deteriorated,” Lord Darzi said.
Despite these challenges, Lord Darzi remains optimistic about the NHS’s future, concluding that while the "NHS is in critical condition, its vital signs are strong."
He pointed out that one of the NHS's greatest strengths lies in the accessibility and visibility of community pharmacy, particularly in serving deprived communities.
However, he raised concerns about the declining access to these services, noting that approximately 1,200 pharmacies have closed since 2017.
Although pharmacies have expanded the range of clinical services that they provide, including blood pressure checks, prescription contraception, and minor illnesses, the total spending on the community pharmacy contract has decreased by 8 per cent, he noted.
He stated that while there is a huge potential for community pharmacy to provide even more value-added services for the NHS, there is a “very real risk” that, if current trends continue, community pharmacies will face access problems similar to those faced by general practice, with “too few resources in the places where it is needed most.”
Community pharmacy welcomes the Darzi report
Pharmacy organisations are hopeful that the report’s findings will prompt ministers to take swift action to tackle the chronic underfunding that is driving pharmacy closures.
Paul Rees, Chief Executive of the National Pharmacy Association (NPA), said: “Lord Darzi’s report must spur Ministers into immediate action to end the scandal of pharmacy closures caused by chronic underfunding over many years, that is eating away at frontline patient care.
“With pharmacies closing at the rate of seven a week and so many more teetering on the brink, the millions who use pharmacies simply can’t wait. They need action now.”
He emphasised that modest investment to ensure adequate pharmacy funding could “transform frontline care, end the scramble for doctors’ appointments, and help fix the NHS fast.”
Community Pharmacy England (CPE) agrees with Lord Darzi’s report that it is absolutely essential to “refocus healthcare towards community and primary care services.”
Janet Morrison, Chief Executive of Community Pharmacy England (CPE) asserted that the investigation report echoes many of the concerns that pharmacy bodies have been raising with policymakers for some time.
“The report’s findings paint a bleak picture of primary care. This is even more so for community pharmacy: we have received less than any other part of the NHS, with a 30% cut in real terms over the last 7 years and a fall in share of the NHS budget from 2.4% to 1.6%.
“The stark financial situation has reached a tipping point, and the degradation of service and risk of collapse is now putting at risk the most basic of the public’s expectations of the NHS – the safety of their medicine supply – critical to the 48% of the population who rely upon their pharmacies for their repeat prescriptions.”
She noted that Lord Darzi’s findings demonstrate “the value of having an accessible pharmacy network supporting people to live well with the medicines they are taking and providing clinical care for patients.”
Malcolm Harrison, CEO of the Company Chemists’ Association (CCA), welcomed the report’s findings and the acknowledgment of the critical state of NHS and community pharmacy.
Harrison highlighted the severe impact of a 30 per cent real terms cut in funding since 2015, which led to the closure of over 1,200 pharmacies.
Despite a shrinking funding pot, community pharmacy productivity has increased, with the number of items dispensed each year growing by over 100m between 2017/18 and 2023/24 and a 115% rise in clinical services delivered in community pharmacies.
Harrison added: “The review rightly points out that there is huge potential to harness the clinical capabilities of pharmacists. Expansion of Pharmacy First, which the report describes as a ‘notable success’ is key – a fully-fledged service could free up 30m+ GP appointments each year.
Similarly, pharmacies can play an even bigger role in administering vaccinations as the report rightly highlights concerns around declining uptake.”
However, he stressed that expanding the roles of community pharmacies can only occur if action is taken to protect the existing community pharmacy network through additional investment.
Harry McQuillan, Chairman of Numark, noted that community pharmacy is the lifeline the NHS cannot afford to lose.
He said: “If access to pharmacy continues to decline, we are at serious risk of replicating the current issues facing general practice – long waiting times, overstretched resources, and a growing number of patients with unmet healthcare needs.”
The Lord Darzi report cited Pharmacy First service as a model of care that could be expanded across the country. McQuillan underscored that “to make Pharmacy First a truly national solution, we need more than just policy recognition; we need real and sustained investment.”
The report indicated that spending on the community pharmacy contract has fallen by 8% since 2015, but McQuillan estimates that, when inflation is considered, that figure rises to a 30% cut.
Combining this with increasing demand and expanded services, McQuillan warned that “a perfect storm is brewing, if it hasn’t already hit.”
He stressed that to truly unlock the potential of community pharmacy, this trend needs to be reversed.
“Sustained and reliable investment is critical if we are to prevent further closures and maintain, and ultimately improve, access to pharmacy services for all communities, particularly those most in need.”
McQuillan asserted that the findings of the Independent Investigation provide the basis for the new Westminster government and policymakers to act, urging them to implement Lord Darzi’s recommendations and unlock the full potential of community pharmacy.
The Pharmacists' Defence Association (PDA) welcomed the Darzi Review, calling it “a very welcome piece of work,” and noted that with a new government in place, there is now “a real opportunity after years of neglect to start to repair the NHS.”
In his report, Lord Darzi stated: “My colleagues in the NHS are working harder than ever but our productivity has fallen.”
Mark Koziol, PDA Chairman agreed, noting, “This is exactly what our members, through focus groups and other forms of feedback have been telling us for years.”
“Consequently, the PDA has consistently argued that the broken system has resulted in everyone working hard but not working smart. This is what the PDA submitted to Lord Darzi while he was preparing his report.”
The PDA has produced a range of strategy and policy papers over the years that have argued for the re-engineering of the system to foster greater integration and collaboration of all healthcare professionals for the benefit of the patient, the NHS, and the taxpayer.
The association stated that their recommendations align with Lord Darzi’s findings which emphasise that, “We need to rebalance the system towards care in the community rather than adding more and more staff to hospitals.”
Lord Darzi noted that restoring the NHS to peak performance will take time.
“It has taken more than a decade for the NHS to fall into disrepair so improving it will take time. Waiting times can and must improve quickly. But it will take years rather than months to get the health service back to peak performance.”
“I have no doubt that significant progress will be possible, but it is unlikely that waiting lists can be cleared and other performance standards restored in one parliamentary term. Just as we in the NHS have turned around performance before, we can do so again,” he said.
Lord Darzi also presented several recommendations for how to repair the NHS, including the need to embrace new multidisciplinary models of care that bring together primary, community and mental health services.
Furthermore, he suggested the health system should tilt towards technology to unlock productivity, highlighting the enormous potential of AI to transform care and the opportunities for life sciences breakthroughs to develop new treatments.
Based on Lord Darzi's report, Prime Minister Keir Starmer has announced plans for "major surgery" to reform NHS.
"What we need is the courage to deliver long-term reform - major surgery not sticking plaster solutions," Starmer said in his major speech at the healthcare charity King's Fund in London.
“My government will always make the investments in our NHS that are needed. But we have to fix the plumbing before turning on the taps,” he said.
Starmer highlighted increased digitisation, reducing the burden on hospitals, and shifting the focus from treatment to prevention as key areas for reform.
















 Health Secretary Wes Streeting addresses Pharmacy Conference via video
Health Secretary Wes Streeting addresses Pharmacy Conference via video 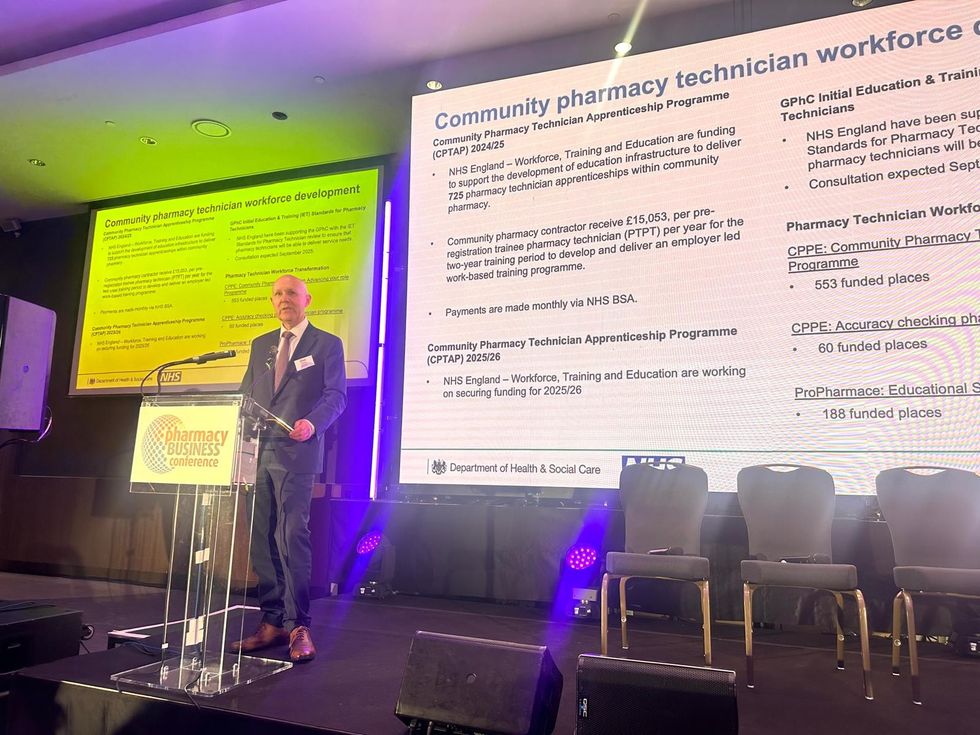 David Webb, chief pharmaceutical officer of NHS England
David Webb, chief pharmaceutical officer of NHS England Shailesh Solanki, executive editor of Pharmacy Business
Shailesh Solanki, executive editor of Pharmacy Business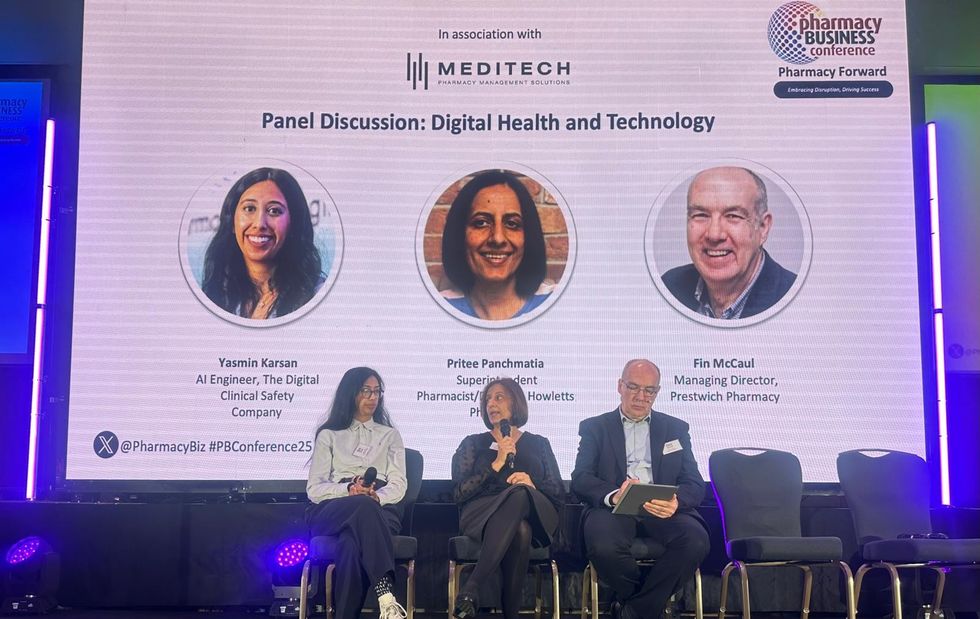 L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul
L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul  L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu
L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu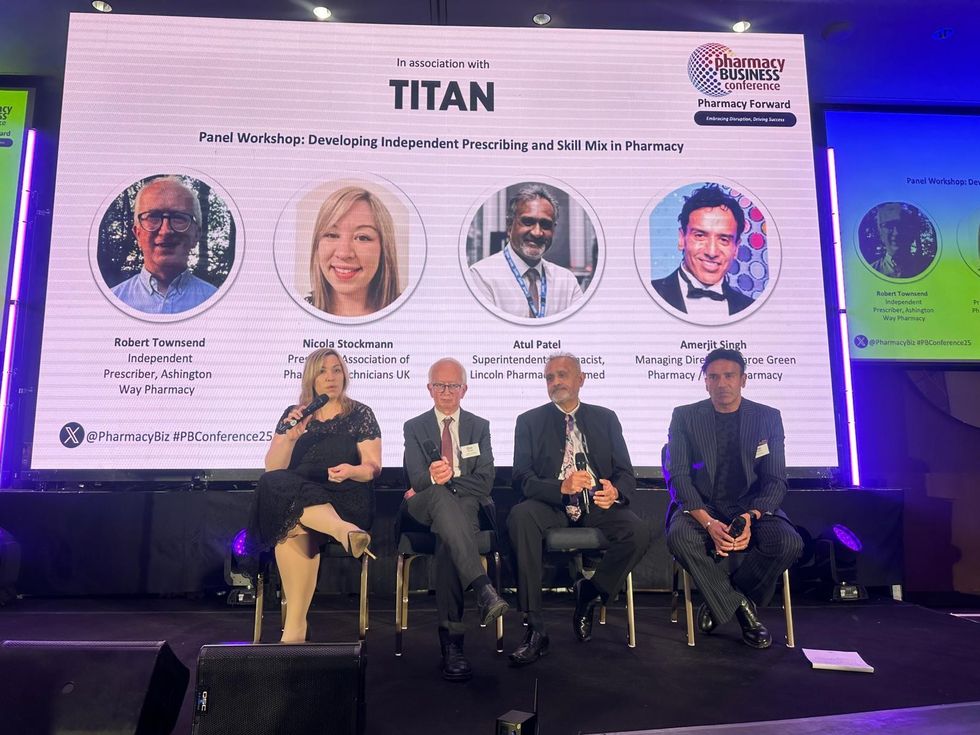 L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh
L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh Wole Ososami, lead pharmacist at Westbury Chemist
Wole Ososami, lead pharmacist at Westbury Chemist

