Harry McQuillan offers insights into Numark’s 12 principles for a future model of pharmacy ownerspharmacy owners practice…
As part of its commitment to enhancing business performance and ensuring safe, effective pharmaceutical care, Numark has developed 12 guiding principles to help its members in adapting to evolving skill sets and shaping their future.
Numark’s future model for community pharmacy practice presents an ambitious vision for the sector, focusing on delivering a range of clinical services, enhancing the health of local populations, and becoming an integrated part of primary care.
Harry McQuillan, Chairman of Numark, reveals that these principles were derived from changes in pharmacy education, such as the integration of prescribing into undergraduate courses.
He views these principles as a formal recognition of the skills that pharmacists and pharmacy teams have developed over time, particularly in the area of independent prescribing.
“These principles formalize those evolving capabilities of pharmacists, especially in independent prescribing,” McQuillan tells Pharmacy Business.
He emphasises the importance of leveraging data and technology to maximize these capabilities and transform the role of pharmacists from responders to active participants in patient care.
“While many people now use smart devices that are capable of recording and sending health data, this information is largely underutilized in both pharmacy and healthcare.
“As that type of technology becomes more dependable, it could offer valuable insights, transforming pharmacists' roles from merely responding to prescriptions to using data as a basis for interventions, including writing prescriptions themselves,” he says.
Future of pharmacy
McQuillan describes their future model of pharmacy as “still grounded and anchored in the communities, with a clear separation between who is involved in the supply and care functions.”
“Technician teams will focus on the accuracy of medicine supply, while pharmacists and prescribers will concentrate on delivering patient care within the same premises,” he explains.
Numark’s12 principles have been shared with Chief Pharmaceutical Officers across the four nations for initial input.
McQuillan says that the responses from two CPhOs have been positive, with more meetings planned to gather further views.
“If someone doesn't agree with the new principles or that direction of travel, I welcome discussion and debate to assess whether adjustments may be needed.”
However, he believes these principles provide a strong starting point for shaping the future direction of pharmacy practice.
McQuillan iterates that the goal is to make the model of future practice “universal, coordinated, and impactful” drawing on the community pharmacy network's strong response during the pandemic.
“During the pandemic, the community pharmacy network played a crucial role in responding to the public health crisis. The network truly came together to ensure the safe delivery of services, keeping patients well at home and maintaining the supply of medicines. Had the NHS community pharmacy network not been in place, the system could have collapsed.”
“I'm confident that if the network agrees on a direction of travel and our capabilities, it can deliver significant public health outcomes. That's why I am keen to at least start the debate on what the future model of pharmacy practice could be.”
Challenges ahead
To effectively implement these principles, McQuillan stresses the need for investment to stabilize the pharmacy network and to improve infrastructure, particularly in technology.
He notes that while many pharmacies already have consultation rooms, investments will be required in technology and infrastructure to fully realize the benefits of the new model.
Acknowledging the disparities in infrastructure across the UK, he anticipates that the principles will be adopted at different paces across the four health systems.
McQuillan notes that England and Wales are ahead of Scotland and Northern Ireland in terms of infrastructure. However, Scotland leads in terms of the structure of service delivery and the range of services provided by pharmacies.
“We have four different health systems that will need to adapt and progress at different paces, and that's okay as long as the underlying principles can be delivered,” he says.
McQuillan asserts that for the government and the NHS to successfully deliver this model of care to their citizens, it is crucial to provide the necessary financial investment.
However, he believes that instead of simply requesting funds and proposing a plan, it's more effective to present a detailed plan and specify the required investment for its delivery.
He notes that, currently, Scotland's financial model supports this type of delivery better than the other three nations. But this could change as perspectives evolve, he says.
The role of technology
McQuillan underscores the significant impact that technology can have on the future of community pharmacy, pointing to scanning technology as a key tool to boost both the accuracy and efficiency of medication supply processes.
“I could see a point where all our patient medication record systems enable accuracy checking using scanning and high-volume pharmacies adopt the hub and spoke model to enhance efficiency.”
“Technology is also going to be necessary to improve efficiency as well as safety as we go ahead.”
“It’s possible to achieve 100% accuracy in the community pharmacy network supply process if we deploy the technology.”
He also sees artificial intelligence (AI) as a valuable tool for supporting clinical checks, such as assessing whether a patient's repeat prescriptions are appropriate, and decision-making by identifying potential issues.
While AI will not replace human judgment, it will augment pharmacists’ ability to make informed decisions, he adds.
McQuillan points to innovative approaches in other countries, such as electronic prescribing and robotic technology coupled to streamlined supply chains in Holland, as examples worth exploring.
In the Netherlands during the late 90s, pharmacists were already using electronic prescribing and robotic technology, allowing them to leave the pharmacy to conduct patient reviews alongside doctors and colleagues from multidisciplinary teams, while the pharmacy continued to function smoothly.
On a recent visit to the Netherlands, McQuillan saw first hand how medicines are assembled and delivered direct from wholesale to pharmacies, ready for supply to the patients, freeing pharmacists for more patient-facing interactions.
Legislative changes required
McQuillan acknowledges that while some legislative changes may be necessary, particularly concerning supervision, most required legislative changes are already in place.
According to him, the primary challenge now is to foster debate within the profession and engage in discussions about potential adjustments.
“But if we agree this is the direction of travel, then those debates become easier,” he notes.
McQuillan advocates for legislation that supports “efficient and safe supply processes to free up pharmacists, allowing them to focus on their clinical and independent prescribing skills.”
Community pharmacy-NHS relationship
McQuillan envisions a closer relationship between community pharmacy and the NHS in the future, with pharmacies becoming a central part of primary care.
He notes that the principles are designed to enhance community pharmacy’s role in accessing and sharing data, participating in decision-making, and managing patient care at home.
McQuillan sees significant opportunities for community pharmacies to improve the management of repeat prescriptions, tailoring them more effectively to individual conditions.
“This is not being done at the moment, but if pharmacies took charge of that, it could improve efficiency across the entire supply chain,” he says.
Pharmacy First service
Regarding the latest trends in the pharmacy sector, McQuillan views the introduction of the Pharmacy First scheme as a crucial step in positioning community pharmacies as the “first point of contact for healthcare” and improving population health.
However, he notes that the distribution of funding for Pharmacy First should be based on current network activity to support its implementation effectively.
McQuillan highlights concerns among some Numark members about meeting the Pharmacy First thresholds. He believes that the measurement methods for these thresholds should be reviewed to better reflect pharmacy activities.
“I don't think pharmacies are lacking in their efforts to achieve it. Instead, the method used to measure progress toward the threshold should be reviewed to make it more representative of the pharmacies' activities,” he says.
Community Pharmacy England (CPE) has requested changes to service specifications to address this issue.
McQuillan says that although this adjustment may not make service delivery easier, it could make the criteria for meeting these thresholds more appropriate.
The introduction of independent prescribing is another major development for the profession, he says, while emphasising the need to focus on how to maximize this opportunity safely.
He explains: “The prescribing model for community pharmacies is different from that of GPs. GPs primarily focus on diagnosing issues and then prescribing treatments, while community pharmacies are shifting towards a model where prescribing will become the primary function, with supplying medications as a secondary role.
“While pharmacies will handle prescribing, we will still rely on our GP colleagues to assist with diagnosis and determining the specifics of a patient's condition. Meanwhile, community pharmacies will focus on optimising medication to control disease states and manage symptoms.”
“This approach presents a significant opportunity for the entire healthcare system to get the maximum use of the pharmacy profession and our principles allow that to happen.”
Looking Forward
McQuillan is optimistic about the future of community pharmacy, provided that the profession embraces and adapts to the proposed changes.
“I see a bright future for community pharmacy if we focus on shaping it and working to make that future a reality,” he adds.
He encourages NHS colleagues to consider these principles when commissioning new services and stresses the importance of government investment to support the delivery of the new model.
Numark plans to support smaller pharmacy owners by providing materials and guidance on implementing the new principles.
McQuillan encourages all pharmacy owners, particularly Numark members, to embrace this direction and adapt to the evolving landscape of pharmacy practice.
He shares that Numark will align its offerings with the new principles and collaborate with NHS colleagues to promote and support these changes.
Numark’s vision for the future of community pharmacy emphasises a transformative shift towards integrated, data-driven, and technology-enhanced practice.
By addressing infrastructure needs, embracing technological advancements, and securing necessary investments, the profession is poised to play a central role in the evolving healthcare landscape.
Numark’s 12 principles include:
- Community Pharmacy teams will improve population health and address increasing healthcare demand as part of an integrated wider health system.
- The community pharmacy network will remain vital to local communities.
- Prescribing and supply can take place from the same community pharmacy premises.
- Pharmacy will leverage data to demonstrate need and value in the identification, development, delivery, and evaluation of services.
- The model can be adapted to meet the needs of each of the countries across the UK
- Pharmacists will fully utilise their clinical expertise, primarily prescribing, to improve patient health.
- Community Pharmacy teams will deliver increasing volumes of services.
- Community Pharmacy will play a wider and more comprehensive role in preventative, urgent and acute care.
- The public will have access to a consistent offer of NHS-funded care across all pharmacies, reserving some local commissioning decisions for local patient needs.
- Supplying medicines will remain a core function for community pharmacies, managed by dispensary staff with a focus on accuracy.
- Pharmacists will be focused on medicines safety
- The adoption of technology will improve safety, efficiency and the delivery of future services to meet patient needs.










 Health Secretary Wes Streeting addresses Pharmacy Conference via video
Health Secretary Wes Streeting addresses Pharmacy Conference via video 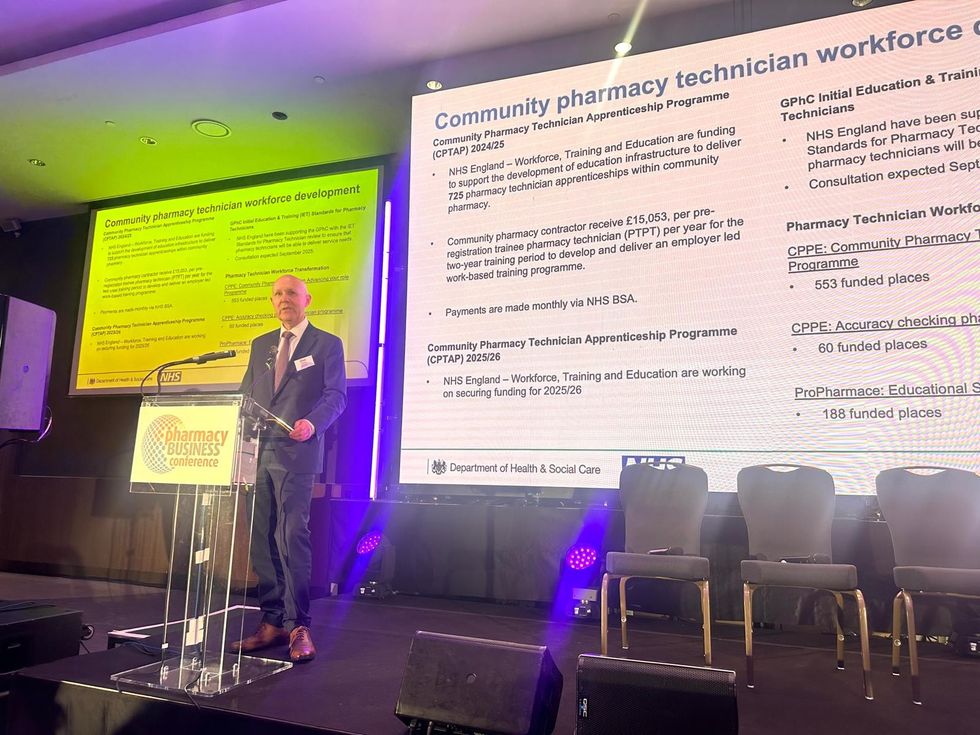 David Webb, chief pharmaceutical officer of NHS England
David Webb, chief pharmaceutical officer of NHS England Shailesh Solanki, executive editor of Pharmacy Business
Shailesh Solanki, executive editor of Pharmacy Business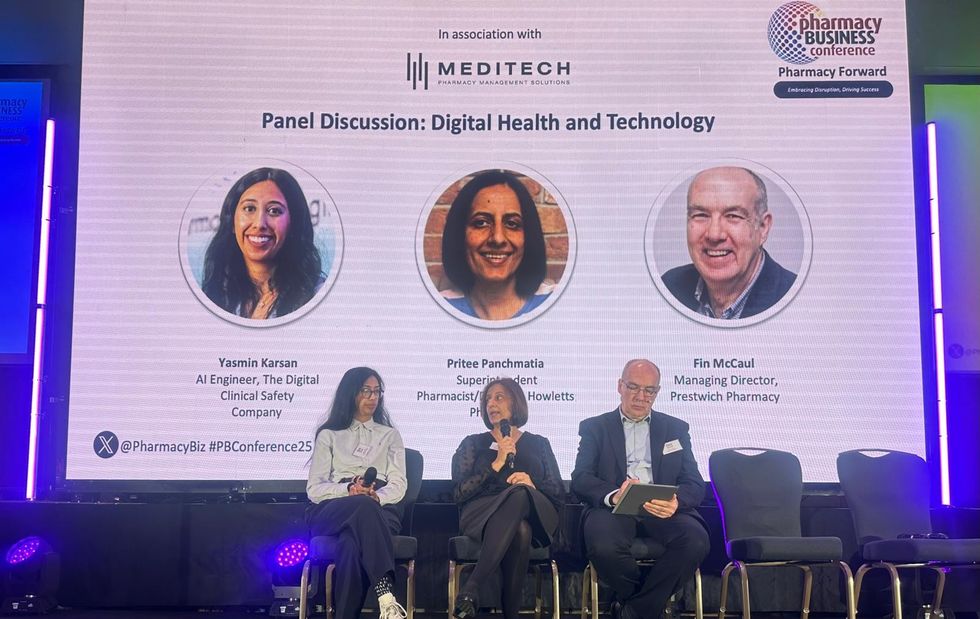 L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul
L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul  L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu
L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu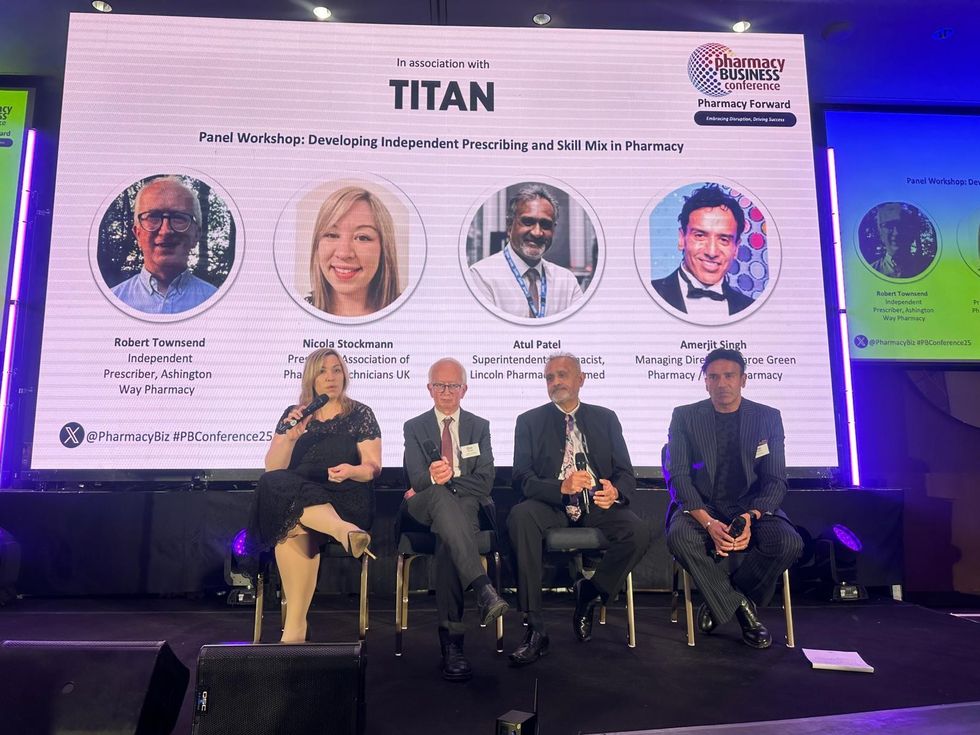 L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh
L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh Wole Ososami, lead pharmacist at Westbury Chemist
Wole Ososami, lead pharmacist at Westbury Chemist








 A woman using kiosk at pharmacy store gettyimages
A woman using kiosk at pharmacy store gettyimages  Pharmacist examining commissioning machine in pharmacy gettyimages
Pharmacist examining commissioning machine in pharmacy gettyimages