Pain Management : Lars-Åke Söderlund outlines non-pharmacological and pharmacological approaches which are currently being used to treat chronic pain…
Pharmacists are a vital member of the multidisciplinary team (MDT) supporting older people to manage their pain. The pharmacist is uniquely positioned to holistically review drug interactions and potential risks associated with each patient’s medication and has the expertise to suggest alternative treatment options to reduce the risks associated with polypharmacy or unwanted side effects caused by other medications.
Chronic pain
The International Association for the Study of Pain defines pain as an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.
Although universally experienced by everyone, the perception of pain is a deeply personal experience influenced by biological, psychological, and social factors, and constitutes an essential behavioral feedback mechanism aimed at protecting us from harm.
Pain may be perceived as either acute or chronic. Chronic pain, defined as pain that persists longer than the normal healing time, constitutes a substantial healthcare burden, affecting approximately 20 per cent of people worldwide and accounts for 15–20 per cent of physician consultations.
Chronic pain is often associated with disrupted mood and sleep, substance misuse and other chronic conditions. Additionally, comorbidities of chronic pain may also lead to complex medication regimens that increase the risks of adverse drug interactions and unwanted side effects.
Treatment approaches
Both non-pharmacological and pharmacological approaches are currently being used to treat chronic pain. Pharmacological approaches for the management of chronic pain include acetaminophen, antidepressants, cannabinoids, gabapentinoids, muscle relaxants, non-steroidal anti-inflammatory drugs (NSAIDs), opioids, and topical analgesics.
Pain is alleviated through diverse mechanisms of action, such as the blockade of pre-and postsynaptic receptors and neurotransmitter release, facilitation of descending pain inhibitory pathways, and through direct targeting of peripheral nociceptors.
The choice of medication used factors in the type of pain diagnosis, recommendations from clinical guidelines, and the patient’s pain medication history as well as personal preferences. Other factors, such as the risk of opioid addiction, or complications due to polypharmacy, must also be considered.
Topical analgesics
Although the systemic administration of analgesics is widespread, topical administration of analgesics has many potential benefits compared to systemic treatment options, particularly for the management of localized and peripheral pain conditions.
This is due to the ability of topical agents to block pain pathways locally or peripherally, with minimum systemic uptake of the topically applied analgesic. Additionally, the lack of systemic drug uptake avoids potential systemic adverse effects and drug-drug interactions, which may be particularly beneficial in patients already on multidrug therapy. It is no surprise that older people are a main target population to benefit from topical agents, and clinical guidelines recommend the use of topical agents for localized neuropathic and non-neuropathic pain.
Additional benefits of topical agents compared to systemic agents include that they usually do not require dose titration, and topical analgesics such as topical NSAIDs, high concentration topical capsaicin, and topical lidocaine constitute a non-opioid option for the treatment of chronic pain conditions such as osteoarthritis and neuropathic or musculoskeletal pain.
Multidisciplinary team
Patients with chronic pain are often treated by a diverse group of medical specialists that collectively form the MDT. An MDT may include neurologists, nurses, complementary therapists, physiotherapists, physical and occupational therapists, dieticians, educational therapists, orthopaedic surgeons, pain medicine physicians, psychiatrists, psychologists, and pharmacists.
Pharmacists may be viewed as more accessible to the outpatient community members of the chronic pain MDT, and have started playing a more active role in the management of patients with chronic pain.
Role of pharmacists
Areas of chronic pain management where pharmacists are increasingly involved include, medication management, the gathering of a patient’s medication history, medication selection, dosing monitoring, deprescribing and discontinuation, evaluation of drug interactions, the management of patients with chronic pain and opioid use disorder, pain education and patient self management, and communication with the wider chronic pain MDT.
Some forms of analgesics, in particular opioids or cannabis, are associated with a risk of addiction, and require careful dose monitoring to maximize the therapeutic effect whilst at the same time minimizing the risk of addition. Additionally, in some geographical regions, pharmacists also routinely provide naloxone kits to patients who use opioids and provide education on how to use naloxone in the event of an opioid overdose.
As chronic pain is often accompanied by comorbidities requiring medication, polypharmacy is becoming increasingly common in the management of chronic pain patients. Increasingly complex polypharmacy may result in both pharmacokinetic and pharmacodynamic adverse drug interactions, and pharmacists are uniquely qualified to identify and address potentially harmful drug interactions.
In particular, pharmacodynamic drug interactions between pain medications and drugs prescribed for comorbid conditions may increase the risk of excessive anticholinergic effects (e.g., muscle relaxants, opioids, tricyclic antidepressants), QT interval prolongation (e.g., methadone, antidepressants, NSAIDs, muscle relaxants), respiratory sedation and death (e.g., benzodiazepines, gabapentinoids, opioids), or serotonin syndrome (e.g., antidepressants, certain opioids, triptans).
As part of this ongoing treatment evaluation, pharmacists should also review each patient’s medication and identify treatments that should be discontinued where appropriate. To facilitate medication tapering or treatment discontinuation of potentially addictive medications such as opioids, guidelines and tools are available to support pharmacists in co-creating a deprescribing plan that will be acceptable for most patients.
Pharmacists may also support patients with behavioral change such as smoking cessation, as smoking has been found to increase pain intensity and lead to greater long-term disability and poorer pain-related functional outcomes in patients with chronic pain.
Due to the, often, complex treatment needs of older people in pain, simultaneous treatment may be administered by different MDT specialists for the management of concurrent physical and mental health conditions.
However, as each specialist may only have a limited overview of medication prescribed by other MDT specialists, the pharmacist is uniquely positioned as a pharmacological treatment gatekeeper, with a holistic overview of the totality of pharmacological treatments offered to each patient, which allows for the evaluation of how multiple treatments may interact with one another.
(Lars-Åke Söderlund is vice president at the International Pharmaceutical Federation or FIP.)








 Health Secretary Wes Streeting addresses Pharmacy Conference via video
Health Secretary Wes Streeting addresses Pharmacy Conference via video 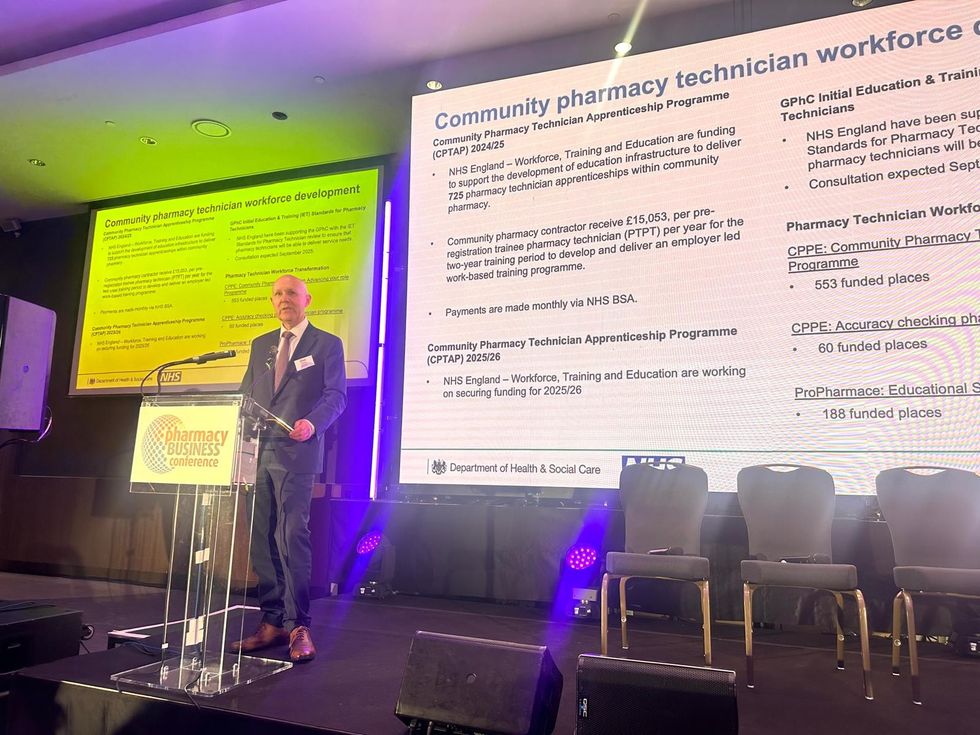 David Webb, chief pharmaceutical officer of NHS England
David Webb, chief pharmaceutical officer of NHS England Shailesh Solanki, executive editor of Pharmacy Business
Shailesh Solanki, executive editor of Pharmacy Business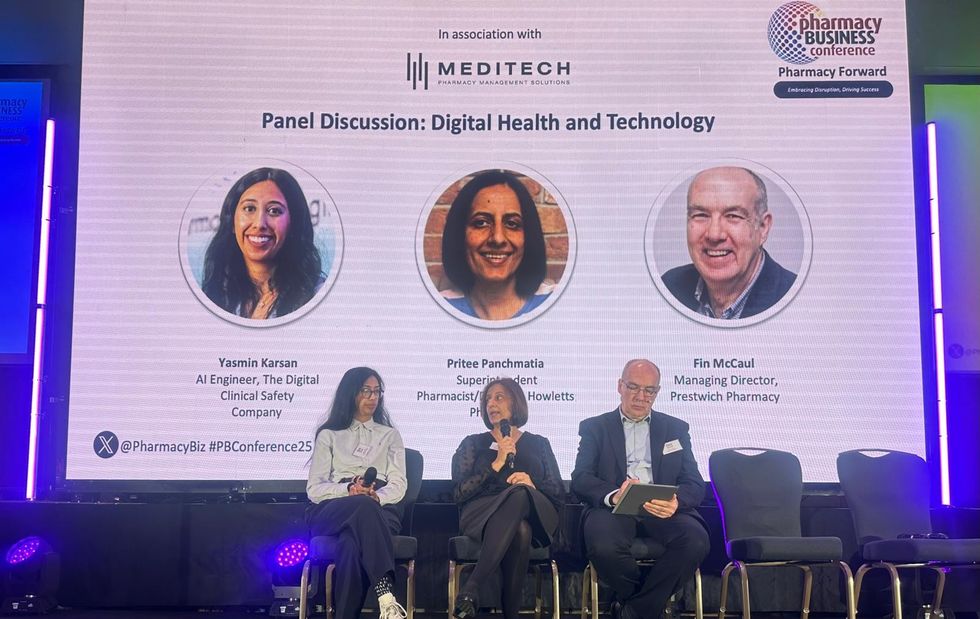 L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul
L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul  L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu
L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu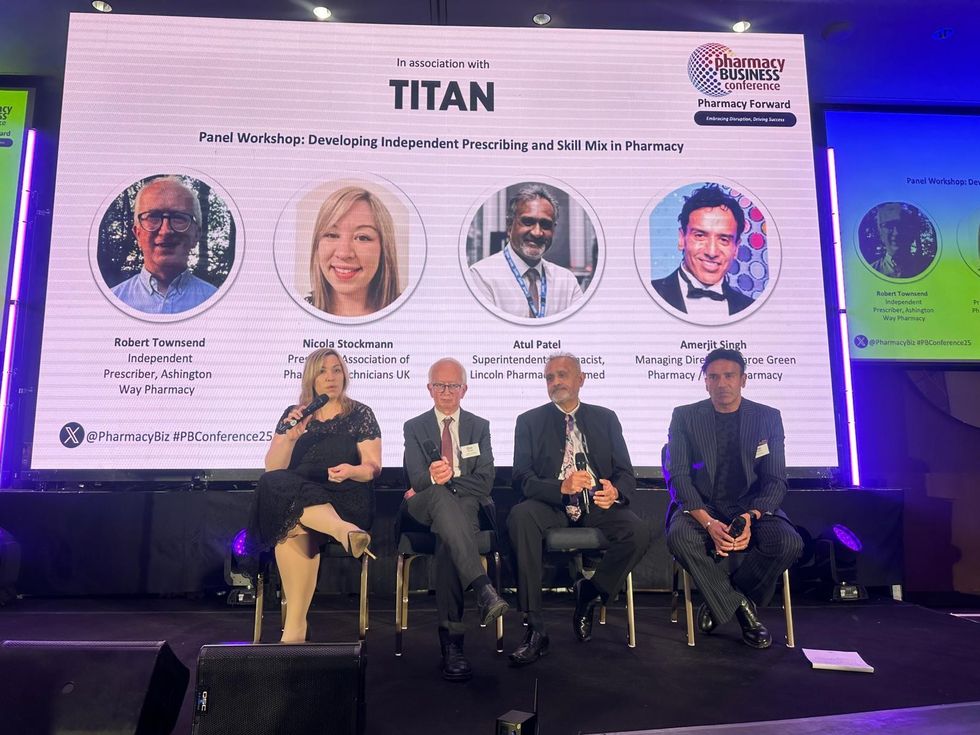 L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh
L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh Wole Ososami, lead pharmacist at Westbury Chemist
Wole Ososami, lead pharmacist at Westbury Chemist








 A woman using kiosk at pharmacy store gettyimages
A woman using kiosk at pharmacy store gettyimages  Pharmacist examining commissioning machine in pharmacy gettyimages
Pharmacist examining commissioning machine in pharmacy gettyimages