Difficulties to book appointments, poor standards of care and distrust in policy-makers are major drivers for dissatisfaction in the healthcare system
The STADA Health Report 2024, published today, has revealed a significant decline in satisfaction with national healthcare systems across Europe, with a notable drop seen in the UK, Germany, and Kazakhstan.
According to the report, satisfaction with the UK's healthcare system dropped sharply by 11 percentage points in just one year, falling from 67 percent in 2023 to 56 percent in 2024. This growing dissatisfaction is likely fuelled by “post-pandemic pressure on the National Health Service (NHS).” In 2020, the satisfaction level was at 85 percent.
In terms of discontentment over healthcare, Britain is followed closely by Kazakhstan and Germany, where satisfaction fell by 10 and 8 percent respectively in one year.
The 10th annual health report released by global healthcare leader STADA Arzneimittel AG, the parent company of Thornton & Ross, is based on a survey of over 46,000 respondents aged 18 to 99 across 32 countries, with around 2,000 respondents in each country.
A continuous decline in satisfaction levels has been observed since 2021. Overall satisfaction with healthcare systems in Europe was recorded at 74 percent in 2020, just before the pandemic. This figure dropped to 71 percent in 2021, 64 percent in 2022, and 61 percent in 2023.
Today, only 56 percent of Europeans feel satisfied with the healthcare system in their country - the lowest figure in five years - as per the report.
Primary reasons for dissatisfaction included difficulties in booking appointments, inadequate care, staff shortages, and a general lack of trust in healthcare policy-makers.
In the UK, 69 percent of respondents cited difficulties in booking appointments as the main reason for their dissatisfaction with the healthcare system.
In Germany, 68 percent of respondents cited appointment booking issues, while in Kazakhstan, 61 percent pointed to the standard of care as a major concern.
Hungary Leads in Dissatisfaction
Overall, Hungary emerged as the country with the highest level of dissatisfaction, with 72 percent of respondents describing their national healthcare system as insufficient. Kazakhstan and Serbia follow closely, with 67 percent and 65 percent of respondents respectively expressing similar concerns.
Across Europe, challenges in securing appointments were particularly pronounced in Hungary (73 percent) while inadequate care was most often reported in Sweden (63 percent).
Trust in health policy-makers is notably low, with almost half of Europeans (46 percent) expressing a lack of confidence in those responsible for health policy. This was the most common complaint in the Czech Republic, where 66 percent of respondents shared this view.
Other reasons for Europeans’ dissatisfaction with healthcare systems included a lack of sustainability (39 percent), the impact of healthcare privatization (30 percent), lack of access to preventive services and shortages of medical staff in hospitals (each noted by 28 percent of respondents.)
Countries with the highest levels of satisfaction
Belgium (85 percent), Switzerland (81 percent), and the Netherlands (77 percent) reported the highest levels of satisfaction with their healthcare systems.
Key factors contributing to this positive sentiment are the availability of medication and good advice from healthcare professionals (doctors or pharmacists). Notably, Germany also scores well in medication availability despite some supply shortages (66 vs 56 European average).
Other factors driving healthcare system satisfaction included the affordability of medication (43), which is rated especially high in Belgium (59), and good access to preventive health services (41), which is particularly valued by the Czech population (62).
The report also noted a correlation between satisfaction with healthcare systems and regular self-care practices. “People who regularly engage in self-care are more likely to be happy with the healthcare system (57) than those who reportedly do little to support their own health (47),” it stated.
How to improve healthcare systems in Europe
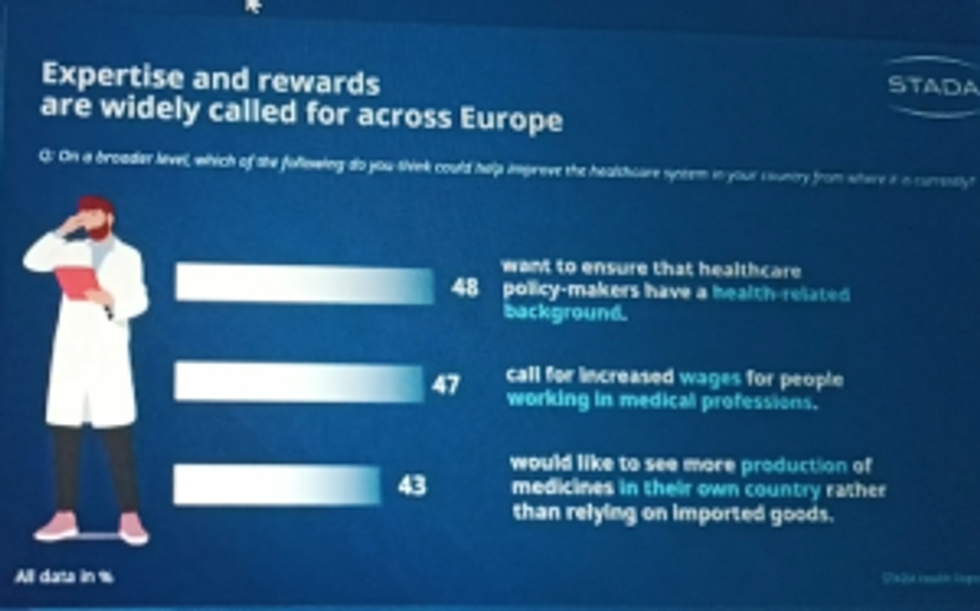
In addition to addressing the immediate causes of dissatisfaction highlighted in the report, the participants suggested several measures to improve healthcare systems in the future.
Nearly half (48 percent) believe that having health policy-makers with a healthcare background would make a positive difference. Additionally, 47 percent advocated for increased wages for people working in medical professions to motivate more people to pursue a career in healthcare, and 43 percent supported increased domestic production of medicines to reduce reliance on imports.
Trust in GPs and pharmacists remains strong
Despite widespread dissatisfaction with healthcare systems among Europeans, trust in healthcare professionals remains strong. General practitioners (GPs) and pharmacists continue to be the primary sources of information for purchasing over-the-counter (OTC) medicines and dietary supplements.
The report also highlighted a rising trust in conventional healthcare among Europeans, with 69 percent of respondents expressing complete or mostly complete trust in conventional medicine – a 7-percentage point increase from 2022.
Men (35 percent) were more likely than women (25 percent) to fully trust conventional medicine.
The main reasons for this growing trust are health practitioners such as doctors and pharmacists. According to the survey, 48 percent of Europeans value their advice, believing that healthcare professionals "know what's best."
Furthermore, 42 percent of respondents trust conventional medicine due to its proven effectiveness, 41 percent place because of decades of research resulting in numerous breakthroughs, and 39 percent cited high-quality standards, regulatory processes, and controls as reasons for their trust.
Those who trust conventional medicine are significantly more satisfied with their healthcare system (59 percent) compared to those who have reservations against conventional medicine (28 percent).
To further improve confidence in conventional medicine, 46 percent of Europeans believe it should focus more strongly on individual patient demands and enhance communication during consultations.
Europeans also desire more medical breakthroughs (41 percent), especially in the treatment of serious diseases such as cancer; a holistic approach to healthcare (40 percent), specialized doctor lists (29 percent), easier access to appointments (28 percent), and more user-friendly medicines (25).
The data also indicated that Europeans are increasingly taking action to care for their health by adopting healthier lifestyles, engaging in more physical exercise, and improving their diets. There is also a growing awareness that physical and mental well-being are equally important.
Peter Goldschmidt, CEO of STADA Arzneimittel AG, said: “I find this trend highly encouraging. I invite all stakeholders—the companies that develop, make and supply essential medicines; the policymakers and regulators who set the frameworks for such products’ use; the doctors who prescribe them; the nurses who administer them; the pharmacists who dispense them; and the patients who benefit from them—to join the debate around the many challenges, but also potential solutions, presented in the 10th edition of the STADA Health Report.”
“Through open dialogue, based on empirical data, together, we build resilient health systems for the years to come. “
The 2024 STADA survey was conducted by Human8 via an online questionnaire in February and March 2024. The survey covered 23 countries: Austria, Belgium, Bulgaria, the Czech Republic, Denmark, Finland, France, Germany, Hungary, Ireland, Italy, Kazakhstan, the Netherlands, Po land, Portugal, Romania, Serbia, Slovakia, Spain, Sweden, Switzerland, the United Kingdom and Uzbekistan.












 Health Secretary Wes Streeting addresses Pharmacy Conference via video
Health Secretary Wes Streeting addresses Pharmacy Conference via video  David Webb, chief pharmaceutical officer of NHS England
David Webb, chief pharmaceutical officer of NHS England Shailesh Solanki, executive editor of Pharmacy Business
Shailesh Solanki, executive editor of Pharmacy Business L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul
L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul  L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu
L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh
L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh Wole Ososami, lead pharmacist at Westbury Chemist
Wole Ososami, lead pharmacist at Westbury Chemist








 A woman using kiosk at pharmacy store gettyimages
A woman using kiosk at pharmacy store gettyimages  Pharmacist examining commissioning machine in pharmacy gettyimages
Pharmacist examining commissioning machine in pharmacy gettyimages