The Pharmaceutical Services Negotiating Committee (PSNC) has criticised the latest general practice funding deal for channelling all investment into primary care through GP surgeries.
In a statement on Friday, PSNC Chief Executive Simon Dukes said it was “a crude response to the much wider problem of rising demand for healthcare and the strain on resources in the NHS”.
The deal “will hardly feel like good news to community pharmacy”, he stressed, adding: “One of the key priorities of the Secretary of State and current Government is prevention. This is a long-neglected area but one which is becoming increasingly important if we are to tackle the rising pressures on all health services. To have an impact, the NHS must start investing in this area through community pharmacies.”
“Pharmacies already see some 1.6 million people every day: investing in services that make the most of these interactions and indeed drive more of them could mean that every person in England is regularly seen by a health professional close to their home, helping them to stay healthy and avoid the need to see GPs and other health services in the first place,” he continued.
The PSNC believes driving pharmacy-roles to the GP practices would negatively impact the community pharmacies.
“It will create yet more demand for pharmacy staff and raise the cost of labour, a position which seems all the more untenable given the complete refusal of the Government and NHS to recognise pharmacies’ costs in delivering their ambitions set out in the Community Pharmacy Contractual Framework (CPCF),” Dukes added.
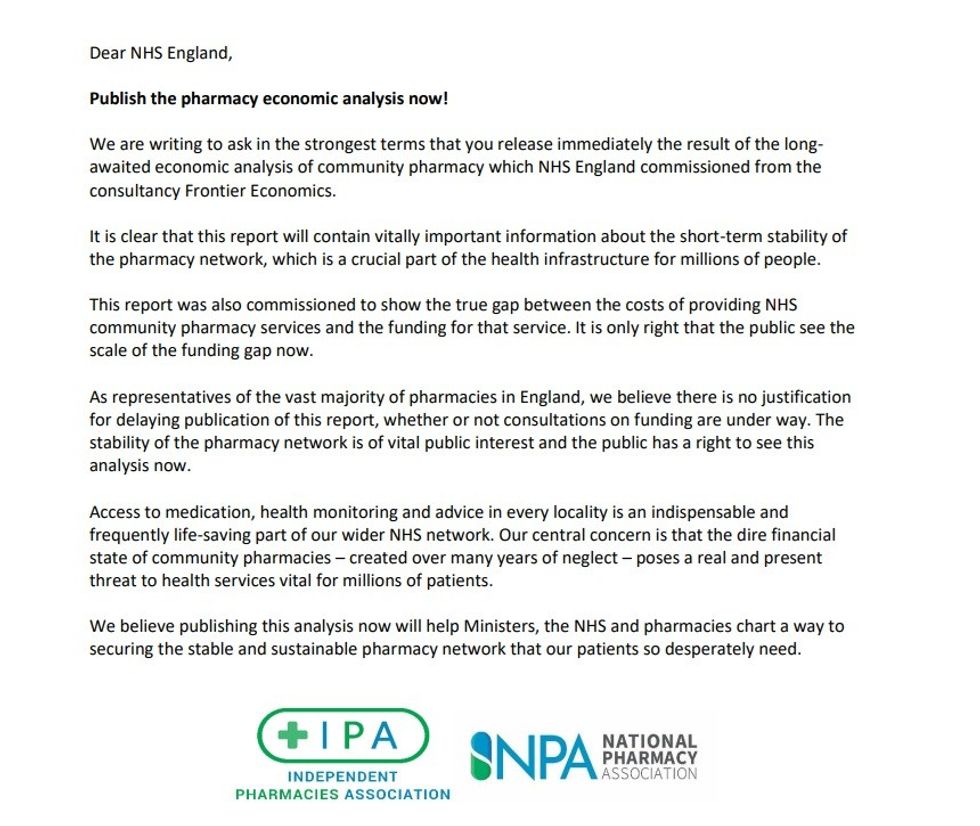
The National Pharmacy Association (NPA) said it "trust that funds can also be found for community pharmacy when pharmacy contract discussions resume".
"With half of all pharmacies in deficit, the government must be prepared to invest in the future of community pharmacy and back us to deliver clinical services to a high standard," NPA said in a statement.
"Primary Care Networks have been told to agree with community pharmacies how they will work together, and this is an opportunity the sector must seize. The ideal outcome would be properly resourced, effective multi-disciplinary care that makes more of community pharmacy premises and the skilled staff employed there. The opposite outcome is possible if PCNs fail to use the flexibilities provided for in this agreement and instead opt for a rigid surgery-based workforce."
Meanwhile, the Royal Pharmaceutical Society (RPS) said that the additional reimbursement showed the importance of pharmacy technicians in the functioning of PCNs.
Claire Anderson, RPS England Board Chair, said: “The RPS had recommended a phased approach to Structured Medication Reviews and the new contract now recognises that delivering them will be linked to pharmacist capacity. We hope the 100 per cent reimbursement will encourage PCNs to recruit into these new roles. The NHS should also consider community pharmacy’s contribution to supporting medicines optimisation and how PCNs can better collaborate across the whole of primary care.”
Anderson stressed the importance of government investment in the education, training and recruitment of pharmacists saying that “PCNs will only be able to move as quickly as the workforce grows and develops”.
“With a potential expansion of the Community Pharmacists Consultation Service, we also look forward to further discussions with the NHS, government and colleagues in the profession on making the most of pharmacy to support patient care,” she added.