Lord Livermore assures that funding has been set aside to protect the public sector's spending power from the direct impact of the national insurance increase
Members of the House of Lords debated the National Insurance Contributions (Secondary Class 1 Contributions) Bill on Monday (6 January) during its second reading.
Lord Livermore, financial secretary to the Treasury, opened the debate, emphasising that the Bill was necessary to “repair the public finances, to protect working people and to rebuild our public services.”
He highlighted the economic challenges faced by the government, including a £22 billion black hole in the public finances and several unfunded commitments inherited from the previous administration.
Livermore stressed the government’s number one commitment is “economic and fiscal stability” and the measures in this Bill would ensure that “not a single penny of day-to-day government spending will be funded by borrowing” within three years.
The Bill contains three key measures:
- An increase to the rate of employer secondary class 1 national insurance contributions from 13.8% to 15%
- A decrease of the secondary threshold for employers—the threshold above which employers begin to pay employer national insurance contributions on their employees’ salaries—from £9,100 to £5,000
- A boost to the employment allowance, more than doubling it from the current £5,000 to £10,500, and expanding the eligibility by removing the £100,000 threshold to benefit more employers.

‘Not to act was not an option’
Lord Livermore acknowledged that these measures would lead to higher contributions for some businesses but reassured the House that “more than half of businesses with national insurance liabilities will either see no change or see their liabilities decrease.”
He further explained that 865,000 employers would no longer pay national insurance, while over one million employers would either pay the same or less than before.
Additionally, all eligible employers would be able to “employ up to four full-time workers on the national living wage and pay no employer national insurance contributions.”
Livermore defended the measures, stating that “not to act was not an option” and these choices were “the only route to putting the public finances back on a stable path, while protecting working people and rebuilding the public services.”
The impact of the changes on pharmacists
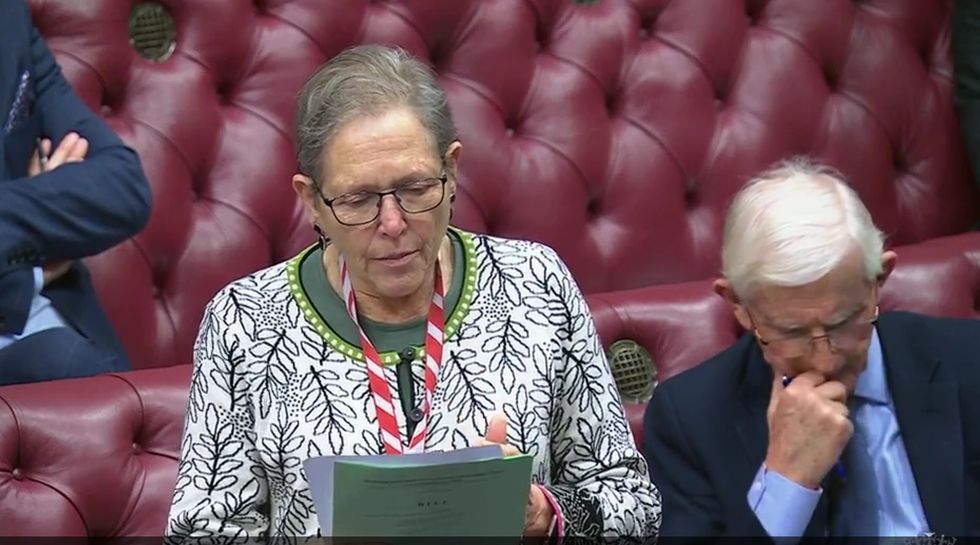
Baroness Kramer (Liberal Democrat) moved a regret motion, arguing that “the Bill risks worsening pressures in the NHS and social care by placing costs on GPs and dentists, social care providers and hospices; increases burdens on small businesses, early years providers, universities and charities; and penalises part-time work, and puts jobs and economic growth at risk”.
Kramer cited their research, which estimated that the national insurance hike will cost GP surgeries some £125.5 million a year, which is equivalent to funding 2 million appointments.
“Hospices, which face a £30 million bill, have warned that they may have to withdraw beds. Research from the Nuffield Trust shows that the cost to adult social care alone will exceed £900 million next year.”
“We risk losing many small care providers and seeing large ones cut capacity. Pharmacists and dentists will not receive compensation in full,” she added.
Baroness Neville-Rolfe (Conservative) and Lord Scriven (Liberal Democrat) highlighted that the new increase in national insurance contributions, as estimated by Community Pharmacy England (CPE), would lead to an additional £50 million annually for the sector.
The National Pharmacy Association (NPA) had cautioned that rising national insurance costs could push small pharmacies into unsustainable financial territory, threatening accessibility for patients.
An NPA survey, conducted before the announcement of the NICs hike, revealed that 72% of small pharmacy owners were worried about their ability to stay afloat in the next five years. The average cost of this increase to a community pharmacy has been estimated at just over £12,000.
Baroness Kramer warned that the knock-on effects will undermine the government’s ambitions to revive the NHS, which in turn will undermine jobs and economic recovery.
In response, Lord Livermore reassured the House that the government has set aside funding, totalling £4.7 billion next year and rising to £5.1 billion by 2029-30, to protect the spending power of the public sector, including the NHS, from the direct impact of the changes.
He added that they are now working with departments to ensure that this funding is allocated appropriately, and that specific funding allocations would be announced shortly.
He also announced that the Department of Health and Social Care (DHSC) will shortly confirm funding for GPs, dentistry and pharmacy.
A "short-sighted" decision
Malcolm Harrison, CEO of the Company Chemists’ Association (CCA), disapproved of the increase in National Insurance contributions, calling it a "short-sighted" decision that will force pharmacies to “stomach the additional costs on top of the 40% real-terms cut in funding they have already been subject to since 2015.”
He argued that pharmacies should either be exempt from paying employers NIC or receive an uplift in funding to account for the added costs.
Harrison also expressed concern over delays in negotiations on the 2024/25 Community Pharmacy Contractual Framework.
“Pharmacies urgently need an uplift in funding if patient access to medicines is to be protected, and further pharmacy closures halted,” he noted.
After the debate, 46 members of the House of Lords expressed support for the amendment, while 61 opposed it, resulting in the amendment being rejected.