A growing number of community pharmacies are closing permanently, mainly due to chronic underfunding and inadequate reimbursement.
Waheedat Owodeyi, owner and superintendent pharmacist at Pharmacyexprezz, said that financial pressures are not exclusive to traditional brick-and-mortar pharmacies—online pharmacies face the same struggles.
Speaking to Pharmacy Business, Waheedat described the current payment structure as "outdated," noting that it has remained unchanged despite advancements in digital systems.
“The way the NHS pays is complicated—you provide a service in January, but you don’t get paid until April,” Waheedat explained.
Adding to the complexity, payments are split into different components. “You receive a small amount at the start of the month—maybe just 10% of what you're owed—then another, unpredictable sum on the 10th. It feels like guesswork,” she said.
“But we have to pay the suppliers at the beginning of every month, which leaves us in debt for those two weeks.
“People say, ‘It’s always been done this way,’ but what may have worked in the past simply doesn’t work anymore—especially now, when there’s hardly any profit left,” Waheedat added.
Another major concern is unsustainable reimbursement rates.
“The government often reimburses less than the actual cost of medicines. For example, they might reimburse £1.50 for a product that costs £2, meaning we’re losing money on every sale.”
“In some cases, losses can be £10–£20 per box, making it impossible to stay profitable, yet the government still expects you to provide medication to patients,” Waheedat noted.
This financial strain has already led to mass closures because a business can’t run on constant losses, she said, adding that “unless negotiations bring real change, this crisis will continue.”
Beyond dispensing, pharmacies provide valuable services but are not adequately reimbursed.
“The government doesn't want to pay for prescriptions because they think that process can be automated—but you still need a human being,” Waheedat noted.
“If dispensing fees are being reduced and we're expected to focus on services, those services must be designed for efficient delivery,” she said, emphasising that the current Pharmacy First model is unsustainable.
Pharmacy First challenges
Waheedat feels that the current Pharmacy First model is difficult to operate efficiently as it creates dependency on others.
She stressed that an efficient online booking platform, similar to those used for COVID and flu vaccinations, is essential for Pharmacy First to reach its full potential.
“I’ve barely completed 10 cases in a year because the service relies on GPs referring patients or individuals seeking us out.”
She proposes a system where patients can directly book Pharmacy First services.
“This would boost patient engagement, reduce GP workload, improve service efficiency, and ensure help pharmacies meet government-imposed targets,” she said.
“The technology is there for them to be able to do it. It's just about them putting everything together to make sure that all these things can be done efficiently,” Waheedat added.
Currently, pharmacies must complete a minimum of 20 consultations monthly—to receive £1,000 at the end of the year.
“Some advance payments were provided, but because I didn’t meet the target, they deducted around £2,000 from me,” Waheedat revealed.
“The issue isn’t that I’m unwilling or unprepared; it’s that I simply don’t have enough patients coming in for the service.
“In contrast, I’ve administered over 12,000–13,000 COVID vaccinations since I started the service in 2021 or 2022, because the system enables patients to find and book the service efficiently.
“The problem with Pharmacy First is that while they’ve introduced the service, they’ve also placed restrictions on it,” she added.
Pharmacies have the potential to take on even more services, but structural reforms are necessary.
Waheedat said: “Negotiations should not only focus on adding more services but also on creating an accessible and functional platform where the patients can choose where they want to go and what service they want to get.
“Instead of penalizing pharmacies for not reaching targets, there should be financial incentives that reward performance—more services provided should mean more funding, not less.”
From March, pharmacists will be expected to provide Pharmacy First, blood pressure checks, contraception services, and more. While pharmacists are willing and ready, the system remains overly reliant on referrals from GPs.
A centralised NHS platform allowing patients to book directly at their preferred pharmacy would be a game-changer, according to Waheedat.
In this video, Waheedat discusses the difficulties in delivering the service...
- YouTubeyoutu.be
The future of pharmacy
Looking ahead, Waheedat envisions a more clinical and accessible pharmacy model where patients receive an expanded range of services.
“Private services hold immense potential—pharmacies will operate like minor ailments clinics,” she predicted.
On the NHS side, she sees inevitable integration.
“Whether now or in a few years, the government will recognise the accessibility and greater potential of pharmacies.
“Pharmacy will play a greater role in screenings, diagnostics, and preventative healthcare, reducing pressure on GPs and A&E.
"Right now, staying afloat is a challenge, but with the necessary support from the NHS, the future looks bright,” she concluded.










 Patricia Tigenoah-Ojo
Patricia Tigenoah-Ojo Baba Akomolafe,
Baba Akomolafe,  Rachna Chhatralia
Rachna Chhatralia Raj Matharu
Raj Matharu


![Potential Side Effects of Mounjaro [What You Need to Know]](https://www.pharmacy.biz/media-library/image.jpg?id=54516976&width=1245&height=700&quality=90&coordinates=0%2C29%2C0%2C29)



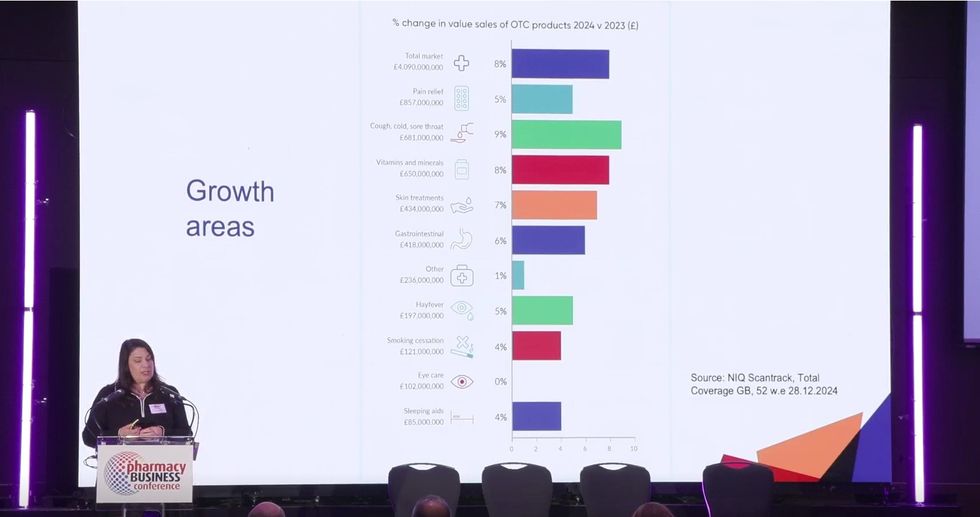 NielsenIQ data shows a positive trend in OTC sales
NielsenIQ data shows a positive trend in OTC sales 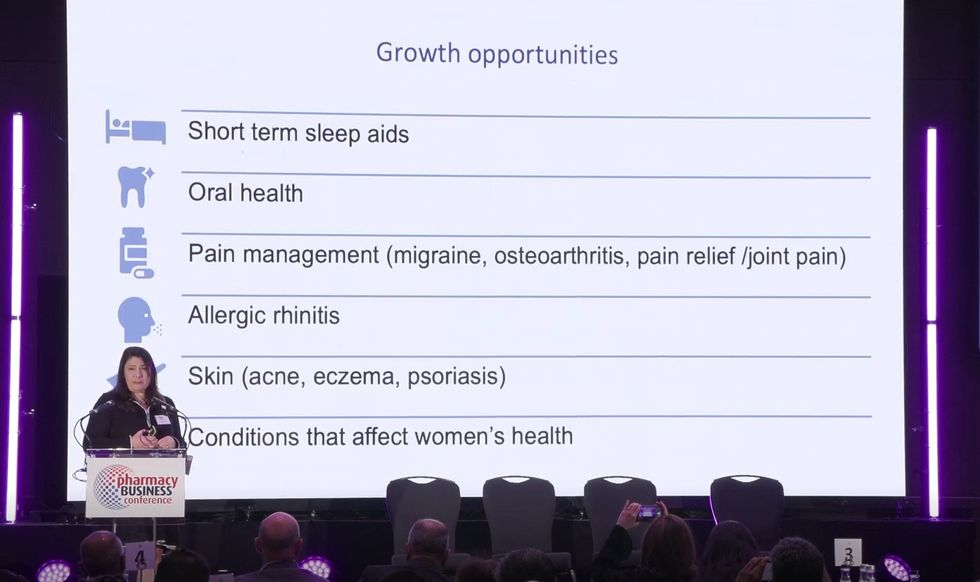 Six broad health conditions where medicines can be reclassified are shown on the screen.
Six broad health conditions where medicines can be reclassified are shown on the screen. 


 Health Secretary Wes Streeting addresses Pharmacy Conference via video
Health Secretary Wes Streeting addresses Pharmacy Conference via video 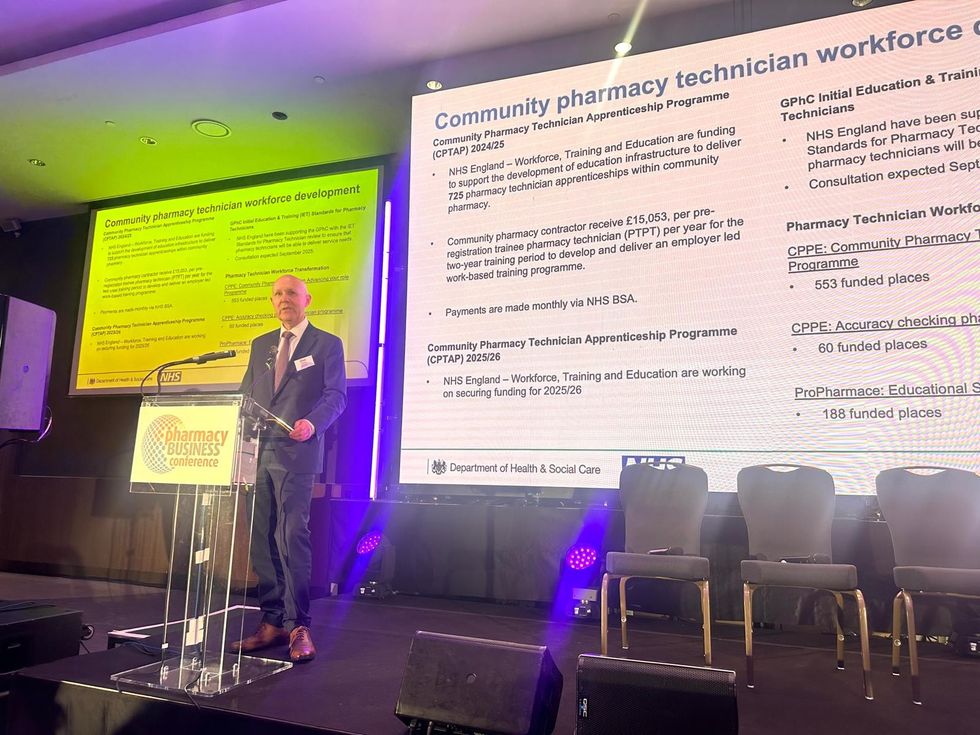 David Webb, chief pharmaceutical officer of NHS England
David Webb, chief pharmaceutical officer of NHS England Shailesh Solanki, executive editor of Pharmacy Business
Shailesh Solanki, executive editor of Pharmacy Business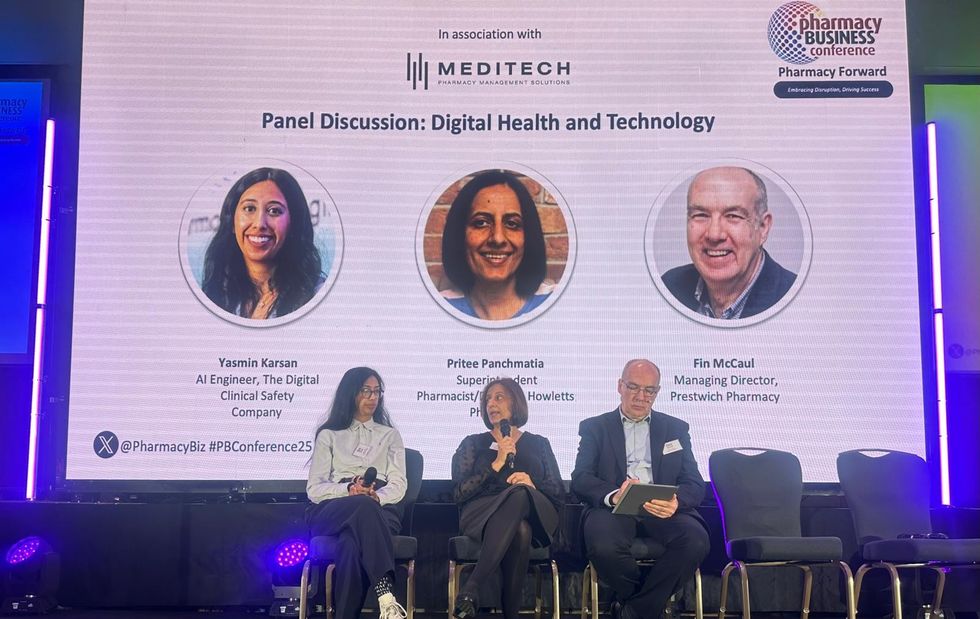 L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul
L-R: Yasmin Karsan, Pritee Panchmatia and Fin McCaul  L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu
L-R: Baba Akomolafe, Rachna Chhatralia, Patricia Tigenoah-Ojo and Raj Matharu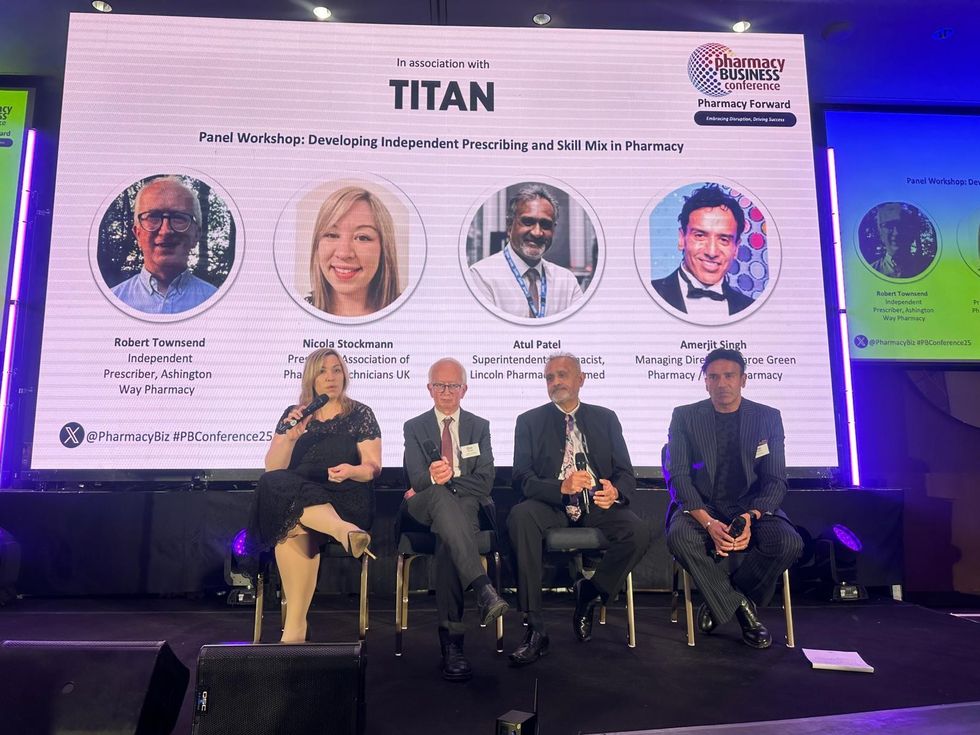 L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh
L- R: Nicola Stockmann, Robert Townsend, Atul Patel and Amerjit Singh Wole Ososami, lead pharmacist at Westbury Chemist
Wole Ososami, lead pharmacist at Westbury Chemist