Former pharmacy minister Steve Brine says investing in local pharmacies to deliver more healthcare in the community will be a highly cost-effective strategy for the NHS…
It has been a hard fifteen months, but I suspect we will look back on 2021 as the Year of the Pharmacist.
I suspect however, for some pharmacists who have been working 16-hour days and struggling to balance the books while keeping their staff safe and serving their patients, it may not feel that way.
The truth is, this awful crisis has allowed pharmacies-who have sometimes been overlooked by the healthcare establishment as fulfilling a vital but limited function – to establish themselves as truly part of the NHS family with much more to offer than just dispensing medicines.
Pharmacies have become the visible face of the NHS during Covid. While most GPs closed their doors, pharmacies stayed open and helped their patients with so much more than just dispensing – providing advice on minor ailments and long term conditions, and becoming a crucial pressure valve to keep patients from overwhelming GPs and A&E departments.
Pharmacists have been no less than heroes, and they have begun to be recognised as such by ministers and indeed the prime minister who have been eager to recognise pharmacists as a true part of the NHS family, something that has not always been the case. With changes at the top of the NHSE executive, this view of pharmacists as so much more than contractors and widget-sellers can only gain more ground.
Pharmacies’ role in the vaccination programme has also been a big step forward for the position of the sector and we heard a positive vision of that role when the minister for vaccine deployment spoke at our first Sigma Taking pharmacy forward webinar.
While it has not been without problems-taking until late February for the NHS to lower the minimum threshold to 400 jabs a week for pharmacy-led vaccination sites – this is a recognition that pharmacies have highly-trained medical staff available on every high street in Britain.
Community pharmacy teams have also administered over a million more flu vaccinations under the national flu vaccination service during 2020-21 than the previous year. If they can do this, what else can pharmacies offer to the community?
This is the crucial question that the sector needs to answer quickly. The promised Health Bill and major reforms to the structure of the NHS – while not the topics that families will be discussing over their summer barbeques – are a window of opportunity for pharmacies to build a new and greater role within the health service.
At a time when the wholly GP-led model of primary care is under unprecedented stress and A&E departments are busier than ever, the network of 11,500 community pharmacies is poised and ready to help, as outlined to me by the National Pharmacy Association which has been the leading voice for community pharmacies during the crisis.
Firstly, pharmacies can play an even bigger role in the general Covid vaccine rollout-allowing GPs to focus on clearing the backlog in the NHS.
Since the outbreak of coronavirus, 68 per cent of the adult population have visited a pharmacy; 35 per cent because a GP had been unable to see them. Local pharmacists are trusted by communities and can help to overcome cultural and communication barriers to vaccine uptake in the most vulnerable demographics.
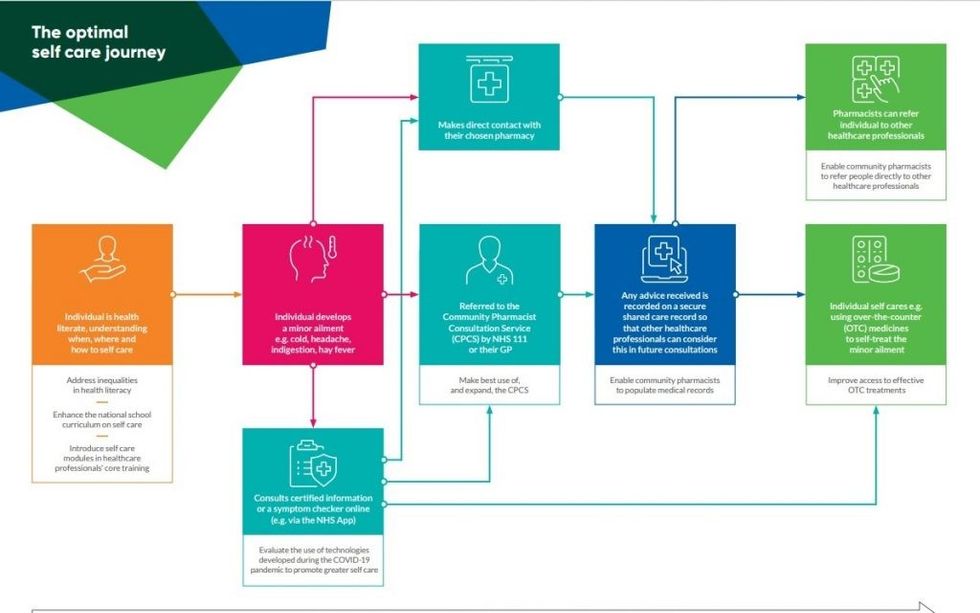
Secondly, pharmacies should be empowered to expand their clinical role through a new service delivery model that will help to take pressure off the NHS, free up capacity in the system and provide greater choice for patients.
Under this model, pharmacies would be the first point of call for many patients, an approach used successfully in many other countries like France where the clinical capabilities of pharmacies are widely recognized to the benefit of the community.
By being positioned as the “front door” to the NHS, they would be able to provide such services as routine management of hypertension, diabetes, asthma and COPD and potentially support for patients with long Covid; medical triage including referrals to GPs and hospitals; provision of initial advice and referral for mental health problems; cardiovascular risks assessments and INR checks; managing patient medicines following discharge from hospital; doing more in care homes… and the list goes on.
This could free up 20 million GP appointments a year.
Pharmacies are also uniquely placed to deliver the NHS’ strategy for prevention, public health, and health inequalities under the newly constituted Office for Health Promotion. Investing in local pharmacies to operate as community health centres is the most cost-effective way to deliver prevention and public health services on the ground.
Maximizing the impact of community pharmacies will depend on sufficient funding as well as strong representation from community pharmacy in the integrated care systems of the future.
Local pharmacies could operate as community health centres, disseminating public health information and helping their patients to prevent and manage the key risk factors such as obesity, excess alcohol intake, high blood pressure, smoking, and poor diet.
Pharmacies can also help to tackle the health inequalities that the government has identified as one of the great moral challenges of our time. More than four in 10 pharmacists come from BAME backgrounds and pharmacies are disproportionately located in the most deprived communities.
For pharmacies to do more, they need to be funded appropriately as the health secretary recognized in his speech to the National Pharmacy Association conference. Pharmacies take a very small share of the NHSE budget and investing in them to deliver more healthcare on our high streets is a highly cost-effective strategy.
And the public is behind this plan. According to a 2020 survey, 81 per cent hold a favorable view of pharmacies; 51 per cent visit their local pharmacy once a month or more; and 78 per cent value a face-to-face relationship with their pharmacist.
Some 84 per cent say NHS should do more to make use of pharmacists’ skills and 71 per cent think pharmacies should expand their offering to take pressure off the NHS.
Pharmacies know they can play a much bigger role in the NHS of the future; the public know it too. Now the sector needs to step up and make it happen.
Steve Brine MP was pharmacy minister from 2017-2019.
















 Graphics courtesy: PAGB
Graphics courtesy: PAGB